Obesity Surgery – Metabolic and Bariatric Surgery
Medical team:
Senior Consultant Privatdozentin Dr. Katrin Kienzl-Wagner (Teamleader)
Senior Consultant Dr. Fergül Cakar-Beck
Senior Consultant Dr. Philipp Gehwolf, MSc, FEBS
Assistant Professor Dr. Heinz Wykypiel, FEBS
Special consultation hours:
Mondays 9:00 a.m. to 3:00 p.m.
Tel. +43 (0)50 504 22511
A-6020 Innsbruck, Anichstraße 35, Building 8, Ground Floor, Outpatient Clinic


Obesity refers to pathological obesity or adiposity. Obesity is a chronic disease and can lead to serious health problems in affected patients due to its accompanying diseases. These comorbidities of obesity include diabetes, high blood pressure, cardiovascular disease, lipid metabolism disorders (hypercholesterolemia), fatty liver disease, degenerative joint disease (knee joint, hip joint, herniated disc), reflux, asthma, and sleep-related breathing disorders (OSAS – obstructive sleep apnea syndrome), polycystic ovary syndrome, and, last but not least, depression.
During our special consultation hours, we provide you with detailed advice on the surgical treatment options for obesity. We prepare you comprehensively for metabolic surgery and offer you close follow-up care after the operation. Both the preparation for the operation, including a detailed assessment, and the follow-up care are carried out in close cooperation with all the specialist disciplines involved, namely metabolic medicine, psychosomatics, dietetics, and plastic surgery. As the patient, you are the focus of our attention. Metabolic surgery can also be performed on adolescents who suffer from obesity and its secondary diseases. In this case, we work closely with the attending specialists in pediatrics and adolescent medicine.
When is obesity diagnosed and who is eligible for surgery?
The key indicator for obesity is the body mass index (BMI). This is calculated using a simple formula based on your body weight and height. (BMI calculator)
According to the definition of the WHO (World Health Organization), obesity is defined as a BMI of 30 kg/m2 and above, with several degrees of severity being distinguished. Surgical treatment of obesity is advisable
– for patients with a BMI ≥ 40 kg/m2
– for patients with a BMI ≥ 35 kg/m2 if one or more obesity-related comorbidities are already present
– for patients with a BMI ≥ 30 kg/m2 who suffer from uncontrollable type 2 diabetes mellitus
In the above mentioned cases, the costs of metabolic surgery are covered by health insurance. However, the procedure must be approved in advance by the respective health insurance provider. Once all the necessary preliminary examinations have been completed, we will send you a letter, that you can use to apply to your health insurance provider for coverage of the costs.
Treatment of obesity
The basis for successful treatment of obesity is lifestyle intervention, i.e., a balanced diet, physical activity, and behavioral measures. There are also medications that can be used to achieve weight loss.
Metabolic surgery remains the most effective method for reducing morbid obesity and curing or alleviating obesity-related comorbidities/concomitant diseases.
What metabolic surgeries do we perform?
The surgeries are performed under general anesthesia. All procedures are primarily performed laparoscopically, i.e., using keyhole surgery. This means that you will have approximately 5 small incisions (5 or 12 mm) in your upper abdomen. Only in exceptional cases is laparoscopic surgery not technically possible, for example if there are extensive adhesions in the abdominal cavity due to previous operations. In this case, a large incision may be necessary.
Sleeve
(Gastric sleeve surgery, sleeve gastrectomy/SG, gastric sleeve, sleeve resection)
Gastric sleeve surgery involves significantly reducing the size of the stomach. To do this, a large part of the stomach is stapled and removed using stapling devices. The remaining stomach then has the shape of a long, narrow tube with an internal diameter of approximately 1.5 cm.
Weight loss after gastric sleeve surgery is based on the fact that, due to the small filling volume of the stomach, you can only consume very small amounts of food. In addition, gastric sleeve surgery changes the release of gastrointestinal hormones, which are responsible for feelings of hunger and satiety and influence the metabolism of food components.
After gastric sleeve surgery, an average weight loss of 50–60% of excess weight is achieved.
Roux-Y Magenbypass

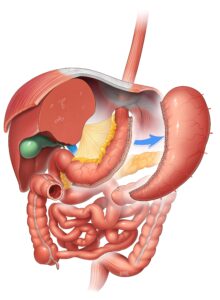
(Roux-en-Y Gastric Bypass/RYGB, classic gastric bypass)
In classic gastric bypass surgery, the stomach is greatly reduced in size, creating a so-called gastric pouch with a filling volume of only approx. 15 ml. This gastric pouch is connected directly to the small intestine. This means that the remaining stomach (stomach remnant), the duodenum, and the upper 150 cm of the small intestine are excluded from the passage of food. Only through a further connection between the small intestine loops are the digestive juices (bile, pancreatic juice) added to the food pulp.
Three mechanisms are responsible for weight loss after gastric bypass surgery: Due to the small filling volume of the gastric pouch, you can only consume very small amounts of food (restrictive effect). Furthermore, by bypassing a large part of the small intestine (the bypass), fewer nutrients from food can be absorbed into your body (malabsorptive effect). In addition, gastric sleeve surgery changes the release of gastrointestinal hormones, which are responsible for hunger and satiety and influence the metabolism of food components.
After classic gastric bypass surgery, an average weight loss of approximately 60%–70% of excess weight can be expected.
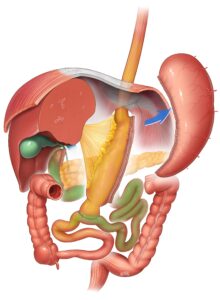
Omega-Loop Magenbypass
(Omega loop gastric bypass/OLGB, One Anastomosis Gastric Bypass/OAGB, Mini Bypass)
The omega loop gastric bypass is a variation of the classic gastric bypass, in which only one anastomosis (= reconnection) is necessary, namely between the stomach pouch and the small intestine.
As with the classic gastric bypass, the omega loop gastric bypass drastically reduces the size of the stomach and creates a gastric pouch with a filling volume of only 15 ml. The remaining stomach, the duodenum, and 150 to 180 cm of the small intestine are excluded from the passage of food. Via the connection between the stomach pouch and the small intestine, the food pulp only comes into contact with the digestive juices (bile, pancreatic juice) after a delay.
The mechanisms responsible for weight loss after an omega loop gastric bypass operation are the same as those for a classic gastric bypass operation. The expected weight loss after an omega loop gastric bypass is comparable to that after a classic gastric bypass operation, and tends to be slightly higher.
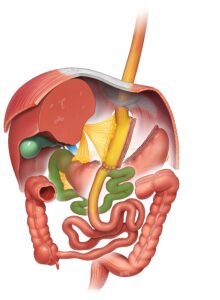
SADI-S
(Single Anastomosis Duodenal-Ileal bypass with Sleeve)
SADI-S is one of the most effective metabolic surgeries. As a result, this surgical procedure is particularly suitable for patients with severe obesity with a BMI > 50 kg/m2.
SADI-S combines sleeve resection (stomach reduction) with an omega loop bypass. In the first step of the operation, a large part of the stomach (approx. 80%) is removed. The stomach remains only in the form of a narrow tube, which drastically reduces the filling volume of the stomach. In the second stage of the operation, a small intestine bypass is created to reduce the surface area for nutrient absorption. To do this, the duodenum is severed immediately after the pylorus and then connected to the lowest section of the small intestine (ileum).
These anatomical changes mean that you can only eat small amounts of food and moreover, the absorption of nutrients and calories is reduced by bypassing a large part of the small intestine. In addition, this operation causes changes in the secretion of gastrointestinal hormones, which reduce the feeling of hunger. After a SADI-S, an average weight loss of 80–85% of excess weight is achieved.
Information material in German
Information material in Englisch
Information material in Croatian
Informatio material in Turkish
Assessment for metabolic surgery
The assessment for metabolic surgery requires several examinations and serves to prepare you optimally for the operation and to select the surgical method that will achieve the best therapeutic success for you.
The first step in the assessment is to attend our patient information event, which takes place every two months. At this information event, you will receive comprehensive information about metabolic surgery. Representatives of the treatment team will give you all the relevant facts and information in the form of short presentations.
Please register for this event via our general surgery outpatient clinic (tel. +43 (0)50 504 22511).
Further assessment then includes examinations at the metabolic outpatient clinic of the University Clinic for Internal Medicine I, an examination at the psychosomatic outpatient clinic of the University Clinic for Psychiatry II, and a dietary assessment.
Furthermore, a gastroscopy must be performed before the operation. If necessary, manometry (pressure measurement of the esophagus) and 24-hour impedance pH monitoring (an examination that measures the presence and extent of gastroesophageal reflux) may also be required.
For referring physicians
Patients who would like to learn more about the possibility of metabolic-bariatric surgery can contact our general surgery outpatient clinic (tel. +43 (0)50 504 22511) to make an appointment to attend our information event.
A preoperative gastroscopy prior to metabolic surgery should be performed shortly before the initial consultation (no older than 6 months) and should address the following issues in particular:
– Assessment of the esophagus with regard to possible reflux esophagitis
– Assessment of the gastroesophageal junction with regard to possible hiatal hernia
– Assessment of the stomach and the visible duodenum
– Routine PEs of the Z-line (4 PEs), corpus and antrum ventriculi (including Helicobacter pylori colonization) and duodenum.